Recurrent Pneumothorax in a Premenopausal Filipino Female: A Case Report
DOI:
https://doi.org/10.70172/pjcd.v22i1.9227Keywords:
lymphangioleiomyomatosis, LAM, pneumothorax, cystic lung disease, progressive dyspneaAbstract
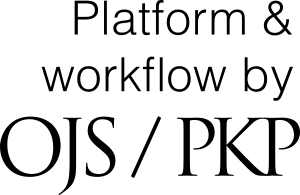
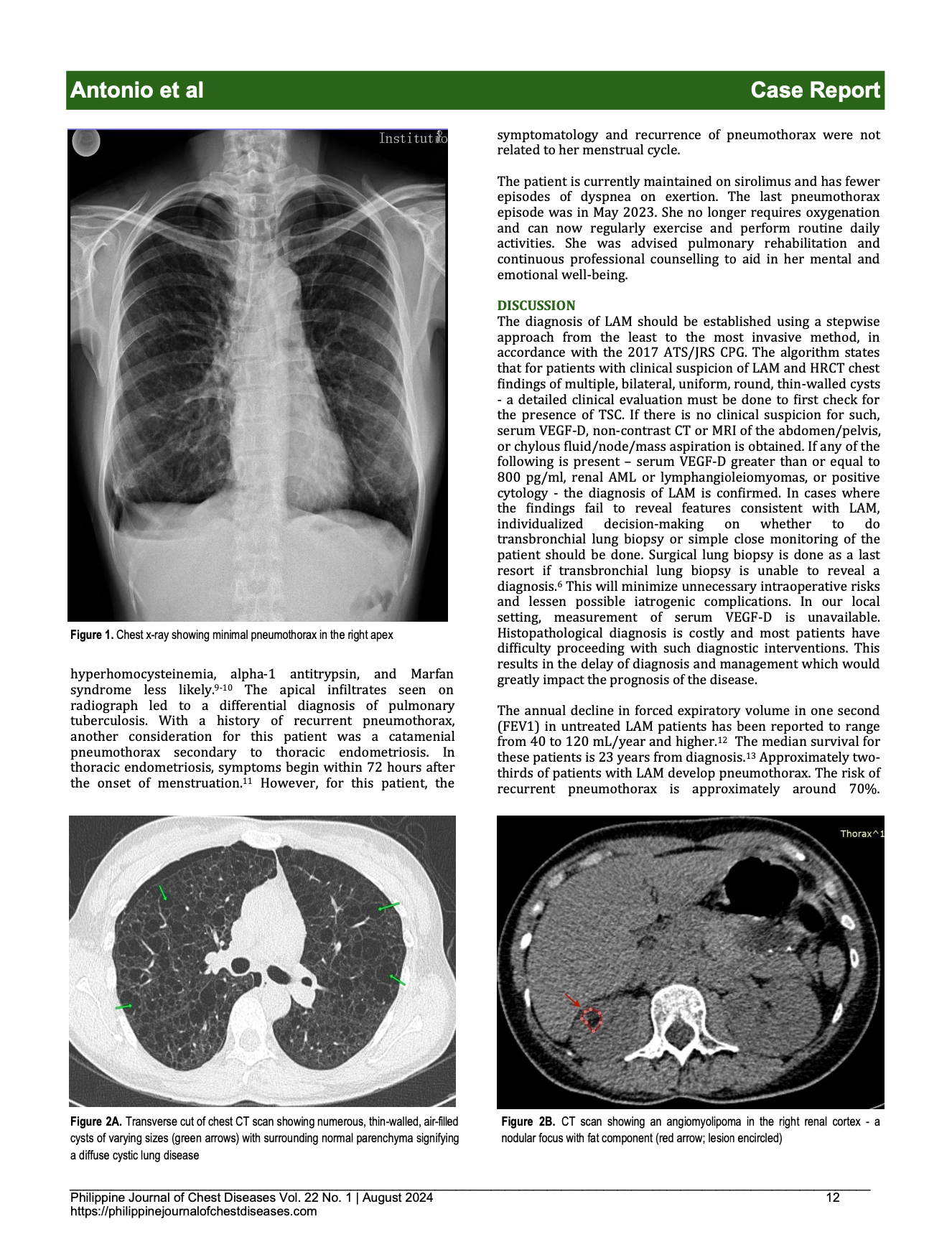
Lymphangioleiomyomatosis (LAM) is a rare progressive multisystemic cystic lung disease. It commonly presents as fatigue, progressive dyspnea, and spontaneous pneumothorax which can progress to chronic respiratory failure. Previously, patients were diagnosed with LAM through histopathological testing. In 2017, new guidelines were released by the American Thoracic Society allowing the clinical diagnosis of LAM. This is the case of a 46-year-old female with a history of recurrent pneumothorax and progressive dyspnea. During episodes of pneumothorax, she underwent multiple chest tube insertions. High-resolution chest CT scan revealed a small right pneumothorax with septations, pleurodiaphragmatic adhesions, minimal pleural effusion, diffuse cystic lung disease, and a fat-containing right renal nodule consistent with an angiomyolipoma thereby fulfilling the clinical criteria for the diagnosis of LAM. The patient eventually underwent talc pleurodesis and was started on sirolimus. LAM should be considered in women of childbearing age without co-morbidities presenting with spontaneous pneumothorax.
References
Johnson SR, Taveira-DaSilva AM, Moss J. Lymphangioleiomyomatosis. Clinics in Chest Medicine 2016;37(3):389–403. https://doi.org/10.1016/j.ccm.2016.04.002 DOI: https://doi.org/10.1016/j.ccm.2016.04.002
Harknett EC, Chang WY, Byrnes S, et. al. Use of variability in national and regional data to estimate the prevalence of lymphangioleiomyomatosis. Quarterly Journal of Medicine 2011;04(11): 971–979. https://doi.org/10.1093/qjmed/hcr116 DOI: https://doi.org/10.1093/qjmed/hcr116
Bispo KA. Recurrent pneumothorax in a patient with a rare case of sporadic lymphangioleiomyomatosis. Philippine Heart Center Journal 2021;24(1):61- 67. Accessed July 13, 2024. https:// www.phc.gov.ph/about-phc/journals/pdf/PHCJVol24_1JanJun2021_CaseReportSeries.pdf
Acero H. Lymphangioleiomyomatosis. Far Eastern University - NRMF Medical Journal 2005;11(1), 25-31. Accessed July 13, 2024. https://registry.healthresearch.ph/index.php?view=research&cid=44015
Pili SF, Espina-Castro C. Lymphangiomyomatosis originating in the uterus. Philippine Journal of Obstetrics and Gynecology 2013;37(2):112-116. Accessed July 13, 2024. https://www.herdin.ph/index.php/partner/journal? view=research&cid=56823
Gupta N, Finlay GA, Kotloff RM, et al. Lymphangioleiomyomatosis diagnosis and management: high-resolution chest computed tomography, transbronchial lung biopsy, and pleural disease management. American Journal of Respiratory and Critical Care Medicine 2017;196(10):1337–1348. https://doi.org/10.1164/rccm.201709-1965st DOI: https://doi.org/10.1164/rccm.201709-1965ST
Cheng YL, Huang TW, Lin CK, et al. The impact of smoking in primary spontaneous pneumothorax. The Journal of Thoracic and Cardiovascular Surgery 2009;138(1):192–195. https://doi.org/10.1016/ j.jtcvs.2008.12.019 DOI: https://doi.org/10.1016/j.jtcvs.2008.12.019
Guo Y, Xie C, Rodriguez RM, Light RW. Factors related to recurrence of spontaneous pneumothorax. Respirology 2005;10 (3):378–384. https://doi.org/10.1111/j.1440-1843.2005.00715.x DOI: https://doi.org/10.1111/j.1440-1843.2005.00715.x
Sattler EC, Syunyaeva Z, Mansmann U, Steinlein OK. Genetic risk factors for spontaneous pneumothorax in Birt-Hogg-Dubé syndrome. Chest 2020;157(5):1199–1206. https://doi.org/10.1016/j.chest.2019.12.019 DOI: https://doi.org/10.1016/j.chest.2019.12.019
Johannesma PC, Reinhard R, Kon Y, et al. Prevalence of Birt- Hogg-Dubé syndrome in patients with apparently primary spontaneous pneumothorax. The European Respiratory Journal 2015;45(4):1191–1194. https://doi.org/10.1183/09031936.00196914 DOI: https://doi.org/10.1183/09031936.00196914
Hwang SM, Lee CW, Lee BS, Park, JH. Clinical features of thoracic endometriosis: A single center analysis. Obstetrics & Gynecology Science 2015;58(3):223. https://doi.org/10.5468/ogs.2015.58.3.223 DOI: https://doi.org/10.5468/ogs.2015.58.3.223
O'Mahony AM, Lynn E, Murphy DJ, Fabre A, McCarthy C. Lymphangioleiomyomatosis: A clinical review. Breathe 2020;16 (2):200007. https://doi.org/10.1183/20734735.0007-2020 DOI: https://doi.org/10.1183/20734735.0007-2020
Oprescu N, McCormack FX, Byrnes S, Kinder BW. Clinical predictors of mortality and cause of death in lymphangioleiomyomatosis: A population-based registry. Lung 2013;191(1):35–42. https://doi.org/10.1007/s00408-012-9419-3 DOI: https://doi.org/10.1007/s00408-012-9419-3
McCormack FX, Inoue Y, Moss J, et al. Efficacy and safety of sirolimus in lymphangioleiomyomatosis. The New England Journal of Medicine 2011;364(17):1595–1606. https://doi.org/10.1056/NEJMoa1100391 DOI: https://doi.org/10.1056/NEJMoa1100391
Xu KF, Tian X, Ryu JH. Recent advances in the management of lymphangioleiomyomatosis. F1000Research 2018;7(F1000 Faculty Rev):758. https://doi.org/10.12688/f1000research.14564.1 DOI: https://doi.org/10.12688/f1000research.14564.1
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 ANa Leandra Antonio, Luzvisminda Ares, Ruby Nolido-Pedroza

This work is licensed under a Creative Commons Attribution 4.0 International License.