Emergence of Candida famata Fungemia in an Immunocompromised Patient: A Case Report Highlighting Clinical Presentation, Diagnosis, and Therapeutic Strategy
DOI:
https://doi.org/10.70172/pjcd.v22i2.9817Keywords:
Candida famata fungemia, immunocompromised host, voriconazole, invasive candidiasis, case reportAbstract
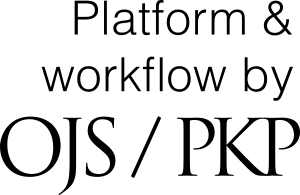
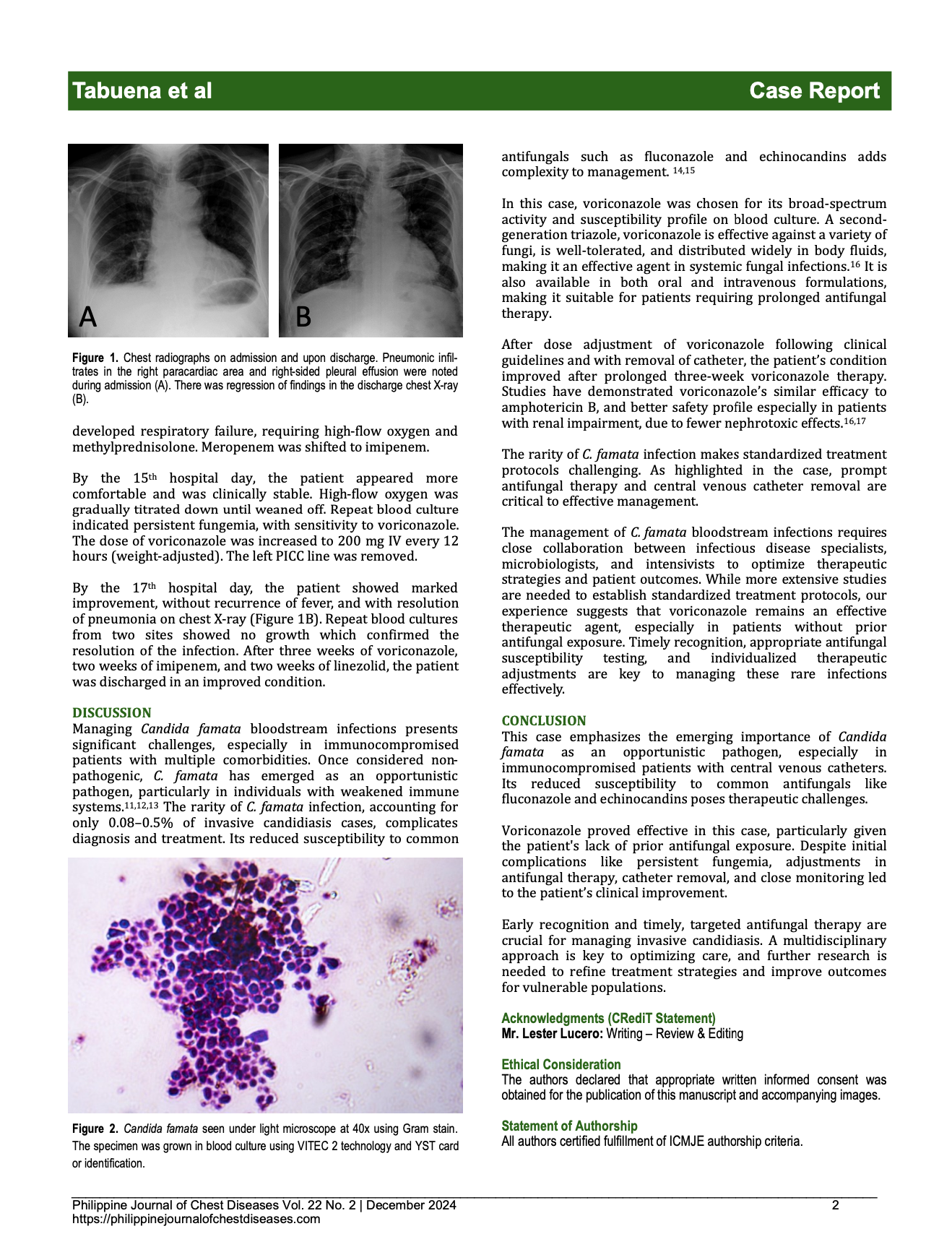
Candida famata, once regarded as benign, is now being recognized as an opportunistic pathogen. This case presents an 88-year-old male with multiple comorbidities who developed C. famata bloodstream infection during treatment for healthcare-associated pneumonia complicated by prolonged catheter use and hospital stay. Antifungal therapy with voriconazole led to clinical improvement and eventual discharge of the patient in stable condition. The rarity of C. famata infection presents diagnostic and therapeutic challenges. This case highlights the importance of timely antifungal therapy and a multidisciplinary approach in managing invasive candidiasis, particularly in immunocompromised patients. Further research is needed to optimize treatment.
References
Voronovsky AY, Abbas CA, Dmytruk KV, et al. Candida famata (Debaryomyces hansenii) DNA sequences containing genes involved in riboflavin synthesis. Yeast. 2004;21(15):1307-1316. https://doi.org/10.1002/yea.1173
Desnos-Ollivier M, Ragon M, Robert V, Raoux D, Gantier J-C, Dromer F. Debaryomyces hansenii (Candida famata), a rare human fungal pathogen often misidentified as Pichia guilliermondii (Candida guilliermondii). J Clin Microbiol. 2008;46(10):3237-3242. https://doi.org/10.1128/JCM.00855-08
Jang YH, Lee SJ, Lee JH, Chae HS, Kim SH, Choe NH. Prevalence of yeast-like fungi and evaluation of several virulence factors from feral pigeons in Seoul, Korea. Lett Appl Microbiol. 2011;52(4):367-371. https://doi.org/10.1111/j.1472-765X.2011.03002.x
Nawange SR, Singh K, Naidu J, Singh SM. Naturally acquired systemic dual infection caused by Candida famata (Debaryomyces hansenii) and Candida catenulata in albino rats bred for sale in the market at Jabalpur (Madhya Pradesh), India. Mycoses. 2010;53(2):173-175. https://doi.org/10.1111/j.1439-0507.2009.01777.x
Al-Hedaithy SS. The yeast species causing fungemia at a university hospital in Riyadh, Saudi Arabia, during a 10-year period. Mycoses. 2003;46(8):293-298. https://doi.org/10.1046/j.1439-0507.2003.00893.x
Beyda ND, Chuang SH, Alam MJ, et al. Treatment of Candida famata bloodstream infections: case series and review of the literature. J Antimicrob Chemother. 2013;68(2):438-443. https://doi.org/10.1093/jac/dks390
Clinical Pharmacogenetics Implementation Consortium (CPIC) Guidelines for CYP2C19 and Voriconazole Therapy. Clinical Pharmacogenetics Implementation Consortium (CPIC). Available at: https://cpicpgx.org/. Accessed October 20, 2024
Badee P, Badali H, Boekhout T, et al. Antifungal susceptibility testing of Candida species isolated from immunocompromised patients admitted to ten university hospitals in Iran: comparison of colonizing and infecting isolates. BMC Infect Dis. 2017;17(1):727. https://doi.org/10.1186/s12879-017-2827-y
Karapetsa M, Tsolaki V, Arabatzis M, Petinak E, Velegraki A, Zakynthinos E. Septic shock due to Candida famata (Debaryomyces hansenii) candidemia in an ICU immunocompetent trauma-patient. Med Mycol Case Rep. 2018;22:69-72. https://doi.org/10.1016/j.mmcr.2018.11.001
Silva S, Negri M, Henriques M, Oliveira R, Williams D, Azeredo J. Candida glabrata, Candida parapsilosis and Candida tropicalis: biology, epidemiology, pathogenicity, and antifungal resistance. FEMS Microbiol Rev. 2012;36(2):288-305. https://doi.org/10.1111/j.1574-6976.2011.00278.x
Deorukhkar SC, Saini S, Mathew S. Non-albicans Candida infection: an emerging threat. Interdiscip Perspect Infect Dis. 2014;2014:615958. https://doi.org/10.1155/2014/615958
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20(1):133-163. https://doi.org/10.1128/CMR.00029-06
García-Effron G, Lee S, Park S, Cleary JD, Perlin DS. Effect of Candida famata (Candida flareri) on susceptibility to amphotericin B and micafungin determined by CLSI and flow cytometric methods. Antimicrob Agents Chemother. 2009;53(5):1617-1622. https://doi.org/10.1128/AAC.01232-08
Pappas PG, Kauffman CA, Andes D, et al. Clinical Practice Guidelines for the Management of Candidiasis: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48(5):503-535. https://doi.org/10.1086/596757
Caria J, Leal E, Dias A, Pinheiro H, Póvoas D, Maltez F. A case of central nervous system infection by Candida famata in an immunosuppressed patient with HIV-1 infection. Med Mycol Case Rep. 2022;38:69-72. https://doi.org/10.1016/j.mmcr.2022.09.004
Klasko S, et al. Voriconazole for Candida bloodstream infections. Antimicrob Agents Chemother. 2005;49(3):1161-1166. https://doi.org/10.1128/AAC.49.3.1161-1166.2005
Kullberg BJ, et al. Voriconazole versus amphotericin B for the primary therapy of invasive candidiasis. N Engl J Med. 2005;352(9):889-890. https://doi.org/10.1056/NEJMe058039
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2024 Rollin P. Tabuena, MD, Shaira S. Arinzol, MD, Ma. Daisy P. Tabuena, MD, Lysa Lynn U. Libanan, MD

This work is licensed under a Creative Commons Attribution 4.0 International License.